When you really immerse yourself in the treatment of a particular area, you begin to pick up on details that you never considered and things that your colleagues continue to miss. This is what happened after I started working at Flex Physiotherapy, with Ian Dowley. Now Ian has worked with only upper limbs for nearly the last decade (so he know a bit on the topic), so as combined our passions, we began to notice a group of patients who were being misdiagnosed with traditional “Tennis Elbow”, although their symptoms were not consistent with our examination findings. It seemed these patients complained of slightly different exacerbating activities and complained of a vague discomfort and weakness in the arm. This article was born from a number of conversations Ian and I had last year resulting in me examining the literature as part of my Masters of Physiotherapy degree. Here is an expanded literature review I completed on – Radial Nerve Entrapment at the Elbow; Radial Tunnel Syndrome and Posterior Interosseous Nerve Syndrome. I hope it allows some insight and better clinical reasoning for your patients with lateral elbow and forearm pain.
Radial nerve entrapment at the elbow is the less well known sister of cubital tunnel syndrome affecting the ulnar nerve and carpal tunnel syndrome affecting the median nerve (Dang and Rodner 2009, Hsu et al. 2012). Radial nerve branch disorders at the elbow fall into two distinct clinical presentations: Radial Tunnel Syndrome (RTS) and Posterior Interosseous Nerve Syndrome (PINS). In both cases the posterior interosseous nerve is entrapped or compressed within the radial tunnel (Lutz 1991). Radial nerve neuropathies at the elbow are considered the rarest of the compressive neuropathies in the upper limb with an annual incidence of 0.003% (Dang and Rodner 2009) accounting for 1-2% of upper extremity nerve entrapments (Cleary 2006).
Identical anatomy is affected in both PINS and RTS, but the symptoms are quite unique. Radial Tunnel Syndrome is characterized by pain or discomfort over the dorsolateral forearm and lateral elbow, with or without pain in the humeral region (Crawford 1984, Kleinert and Mehta 1996, Tsai and Steinberg 2008). Patients with RTS report pain or discomfort as their main complaint, rather than weakness (Tsai and Steinberg 2008, Berton et al. 2012).
Posterior Interosseous Nerve syndrome is characterized by initial lateral forearm pain that progresses to neurological weakness of the ulnar wrist extensors, thumb extensors, finger extensor group (Tsai and Steinberg 2008, Bolster and Bakker 2009) and the supinator (which I’ll discuss later). However, it has also been reported that PINS may develop in absence of pain (Hsu et al. 2012).
There is some confusion in the literature regarding the classification of the radial nerve disorder at the lateral elbow as either RTS or PINS (Hazani et al. 2008). It seems that this is due to the inconsistency in nomenclature of the radial nerve branches in the elbow and forearm region, but a bit more on that later.
Pathology
Pathoanatomy
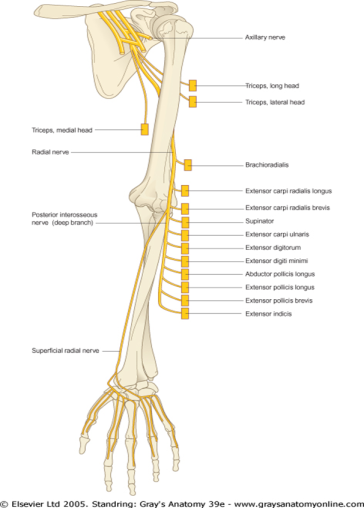
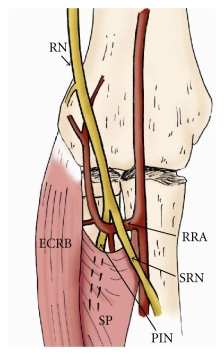
The radial nerve travels distally from its origin at the posterior cord of the brachial plexus, carrying fibres from nerve roots C5-T1. It transverses posterior to the axillary artery, and then transverses the posterior humerus in the radial groove. Approximately 10-12cm proximal to the lateral epicondyle the radial nerve passes through the intermuscular septum separating the posterior and anterior brachial compartments. It continues distally between the brachialis and brachioradialis musculature. Roughly 3-4cm proximally to the supinator muscle, the radial nerve branches off becoming the DBRN and SRN (Dang and Rodner 2009, Hazani et al. 2008).
The current confusion in the literature on this topic of RTS vs PINS is likely related to the anatomical nomenclature of the region. The deep branch of the radial nerve IS NOT the posterior interosseous nerve! Only once the DBRN exits the supinator muscle at its most distal portion is it then named the PIN, approximately 7.5cm distal to the radiohumeral joint (Hazani et al. 2008). I believe this distinction is critical to rationalise the differences in presentation between patients with RTS and PINS. In clinical practice, there seems to be some overlap between these two conditions and I believe this is the case as the pathology is likely a continuum or spectrum pathology.
Diagnosis would therefore likely be dependent on three factors including:
- The variations in the muscular neural innervation
- Location of the nerve compression affecting the motor branches distal to the site of compression
- The degree of nerve compression

The radial tunnel is the site of nerve compression in both RTS and PINS. The tunnel extends from the level of the radiohumeral joint to distal border of the supinator muscle. It is bounded posteriorly by the radiohumeral joint capsule and the deep fibres of supinator; laterally by brachioradialis, extensor carpi radialis longus (ECRL) and brevis (ECRB); medially by the brachialis and biceps tendons; and anteriorly by brachioradialis, brachialis and the superficial fibres of supinator (Berton et al. 2012). Before entering the radial tunnel as the PIN, the radial nerve innervates the ECRL and proximal supinator.
There are five potential entrapment sites of the PIN in the radial tunnel, with the acronym FREAS used to remember them. Listed from proximal to distal:
1) Fibrous tissue bands – between brachialis and brachioradialis at the level of the radiocapitellar joint
2) Recurrent vessels of the radial artery at the radial neck – aka: the Leash of Henry
3) Extensor carpi radialis brevis leading edge – between ECRB and supinator
4) Arcade of Fröhse – the fibrous proximal edge of the superficial fibres of supinator
5) Supinator muscle distal edge
(Tsai and Steinberg 2008, Dang and Rodner 2009).
The Arcade of Fröhse is considered the most common site of DBRN compression. A large proportion of people have a thick, tendinous edge of the supinator muscle at the entry point of the DBRN. Berton et al (2012) performed a brief review of the literature, and reported a wide range (32-87%) of this finding amongst 12 studies. So it seems this may just be a common finding anyway! The studies reported in this review article did not necessarily use live people, with related symptomatic complaints!?! Further surgical studies on live patients may assist to determine if this finding is relevant.
So, if the incidence of a lateral elbow radial nerve branch compression is so low (0.003%), then the large percentage of people with this finding just doesn’t make sense! Based solely on this finding of a thickened edge, you might consider this only part of the puzzle thus far. The other four areas might be also part of the puzzle, but literature is scarce on the incidence of these findings in the surgical rather than cadaveric literature.
The other location most often implicated in RTS and PINS is the tendinous edge of ECRB, which compresses the PIN in actions such as gripping an object in full pronation and isometric wrist extension. The remaining three areas listed are far less common and suffer from the same gaps in the literature regarding the association between symptoms and anatomical findings.
Dare I say, this does not really matter anyway. The pattern of functional loss and correlation with symptoms must be the focus of examination, diagnosis and management. Knowledge of the possible anatomical causes should be understood to help correlate symptoms with location of the nerve ‘dysfunction’. But I don’t get lost thinking about where in the radial tunnel the nerve may be a bit upset, but rather, looking at what modifies their symptoms initially and returns to them to function later.
I believe this approach better suits the current evidence base, as the anatomical variation in this region is so high. It is highly likely that we are unable to yet examine the smaller terminal branches and small diameter afferents of the DBRN and PIN with any current imaging or electrodiagnostic techniques.
Of course, as with any musculoskeletal disorder, you must be aware of other potential precautions and red flags that may mask themselves as a mechanical cause of pain such as lipomas, ganglia, subluxation or fracture of the radial head or synovitis associated with rheumatoid arthritis (Dang and Rodner 2009, Naito et al. 2013)
Pathophysiology
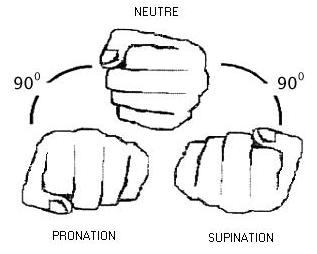
Nerve compression results in alteration of microvascular function and resultant change in nerve and local environment structure. This results in dysaesthesias that progress to motor and reflex loss distal to the compression site (Rempel et al. 1999). The pressure in the radial tunnel has a normal value of 40-50mmHg (Spinner 1968, Werner et al. 1980). Frank peripheral nerve ischemia can occur at pressures as low as 60-80mmHg (in rats) (Rydevik et al. 1981) and axonal transport can be impeded in peripheral nerves from pressures as low as 50mmHg (Bentley and Schlapp 1943). There seems to be little buffer in the normal pressure values before ischemia and axonal transport is altered! The pressure increases rapidly in the radial tunnel to as high as 250mmHg with passive pronation of the forearm (Spinner 1969, Werner et al. 1980).

Frank reductions axoplasmic flow would account for losses of strength observed in PINS. What we don’t yet know is why some people present with a conduction (motor loss) in PINS and why others with RTS present with pain symptoms only. Perhaps it represents the difference in location of the nerve compression and the part of the branch of the radial nerve that is affected (DBRN vs PIN). Perhaps it is due to individual variations in neural innervation or the degree of nerve compression? These are all potential factors, but currently there is no evidence for any of this except good clinical reasoning and basic anatomical science.
There is a widely held belief that the PIN is a motor only nerve (Lin et al. 2006). However there are some interesting basic science studies that have reported that the PIN also houses Type IIA (Ferdinand et al. 2006) and Type IV afferent nerve fibres (Dang and Rodner 2009) which have been associated with nociception. These reports of afferent nerve fibres in the PIN suggest a possible cause of the pain of RTS, as the result of compression of what in the past was thought to be a motor-only nerve. As small diameter afferent neurons are not able to be examined with current electrodiagnostic techniques, there currently no good measure of if input to the CNS from these nerves is relevant in our patients with this disorder.
Patient presentation
RTS and PINS have been described as repetitive overuse disorders of the forearm (Dang and Rodner 2009). In observational studies, those who perform repetitive pronation and/or supination the forearm (Lutz 1991), or sustain these movements in full elbow extension (Roquelaure et al. 2000) are at higher risk of developing these conditions. This includes bartenders, violinists, swimmers (Dang and Rodner 2009), and homekeepers (Berton et al. 2012).
Patients with RTS predominantly describe a vague, deep aching and tiredness in the dorsolateral forearm (Toussaint and Zager 2008, Tsai and Steinberg 2008). Repeated activity involving pronation and supination exacerbates symptoms, and increased pain at night has also been reported (Tsai and Steinberg 2008, Bolster and Bakker 2009).
Patients with PINS describe a weakness in the affected arm, particularly with gripping activities. In severe cases there may be a complete loss of active finger and thumb extension. The loss of strength is usually the primary complaint, with no pain or only mild pain reported (Dang and Rodner 2009). While these are the weakness patterns documented in the literature, clinical experience has shown that the supinator muscle can also be affected. The anatomy within the radial tunnel has considerable variation, and although the supinator is innervated quite proximally within the radial tunnel, its neural branches also have the capacity to be compressed, resulting in supinator weakness.

From: http://www.vwa.vic.gov.au
Patients seem to have difficulty explaining their pain distribution with both types of radial nerve compression, in PINS, they report vague weakness signs, clumsiness or lethargy of the forearm or entire arm distal to the shoulder. Keep an eye out for any symptoms that don’t quite fit a standard pattern of Lateral Epicondylalgia (tennis elbow) or Common Extensor Tendinopathy. Keep in mind that if RTS and PINS lie on a spectrum or continuum, dependent on the degree and location of nerve compression, some patients won’t be so easily classified. Further, based solely on the underlying anatomy, it would make sense that compression of the PIN results in weakness symptoms, while irritation of the DBRN results in RTS, with no true weakness.
The patients presenting to our clinic work quite a bit with their hands, such as cleaners, personal care assistants and tool workers. They typically present with other primary problems, such as pain in the radial sided of the wrist (DeQuervains, sprain), or shoulder that has preceded pain in the lateral forearm. Quite often these patients have undergone surgery in the wrist in the area served by the Superfical Radial Nerve (trapeziectomy, scaphoid fracture) or in the shoulder for a rotator cuff repair, proximal/distal biceps repair or acromioplasty. Associated pain may also be reported in the dorsal wrist and hand, lateral epicondyle and humeral regions (Crawford 1984, Lutz 1991).
Examination
Unfortunately there are currently no objective testing procedures that have been assessed for reliability. A number of authors have described various palpation, pain provocation testing, strength assessment, sensation testing, and imaging techniques are combined to determine diagnosis of RTS or PINS. Clinically in our clinic, we use additional test including grip strength assessment and neural tissue provocation testing.
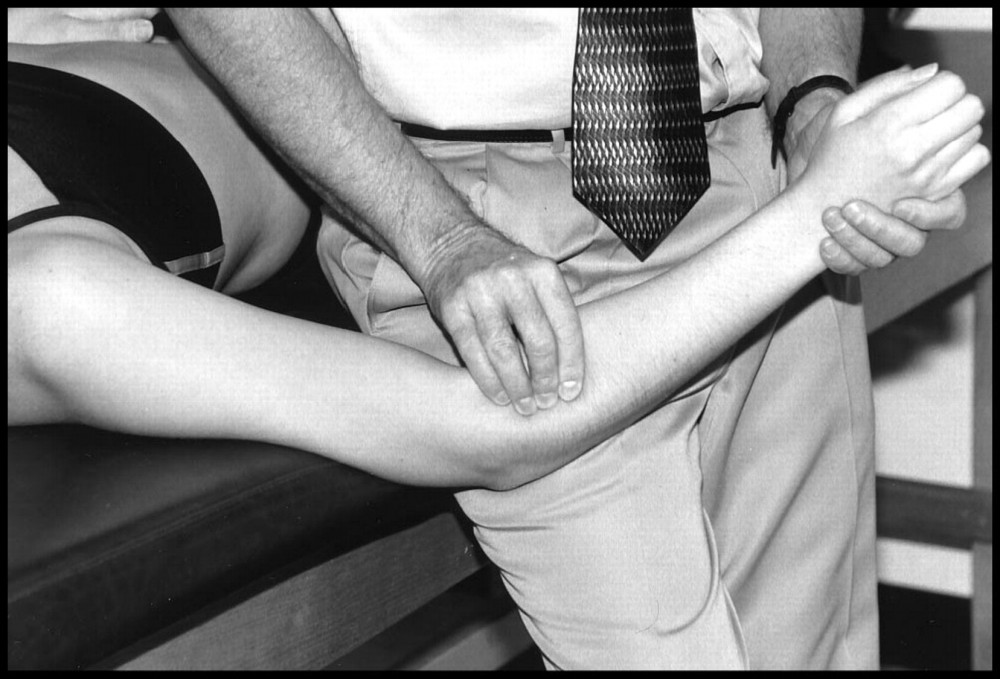
Provocation Palpation
The location of tenderness on palpation is thought to be significant in distinguishing RTS and PINS from lateral epicondylalgia. The primary tender site for RTS and PINS is over the radial tunnel, anterior to the radial neck, near supinator and the medial border of brachioradialis (Lutz 1991, Hsu et al. 2012), whereas the primary tender site in lateral epicondylalgia is located on the lateral epicondyle of the humerus (Huisstede et al. 2006). However, findings may be mixed, as approximately 5% of those with lateral epicondylalgia also have RTS, and 50% of those with RTS also have lateral epicondylalgia (Tsai and Steinberg 2008). Based on clinical experience, most of these patients will also have tenderness over the radial nerve at the lateral intermuscular septum of the arm, and/or near the anatomical snuffbox housing the superficial radial nerve.

Resisted muscle testing – Provocation
Resisted wrist extension and middle finger extension are typically painful in lateral epicondylalgia, but will cause only mild to moderate pain in RTS, and little or no pain in PINS (Tsai and Steinberg 2008, Hsu et al. 2012). Pain during resisted supination indicates RTS, or lateral epicondylalgia (Dang and Rodner 2009) and perhaps PINS. Resisted supination testing in PINS does not normally result in much pain compared to RTS and sometimes lateral epicondylalgia.
Resisted muscle testing – Weakness
To differentiate RTS from PINS and RTS from lateral epicondylalgia, pain inhibition weakness should be considered. Typically, resisted testing in RTS does not elicit weakness symptoms, with pain being the primary complaint on these tests. In PINS and lateral epicondylalgia resisted forearm supination, middle finger extension and wrist extension are the weak movements on testing (Dang and Rodner 2009). Severe weakness, largely in absence of pain is observed more in PINS whereas, in lateral epicondlylalgia weakness and pain occur concomitantly. It should also be noted that in PINS, ECRL is active during resisted testing of wrist extension as it is innervated by the radial nerve before it enters the radial tunnel (Lutz 1991), resulting in an ulnar bias when the wrist is extended. The clinician should also consider testing for proximal nerve involvement assessing for denervation weakness and sensory symptoms due to proximal radial nerve, brachial plexus or cervical nerve root compression which may masquerade as an entrapment neuropathy at the elbow (Tsai and Steinberg 2008). Further, extensor tendon rupture should be considered as a differential for suspected PINS weakness (Dang and Rodner 2009).
Sensation
Cutaneous sensation is not affected in PINS or RTS as the PIN does not have a cutaneous distribution. Other conditions such as proximal radial nerve, SRN, C6 or C7 neuropathies should be investigated as a differential diagnosis (Dang and Rodner 2009). Clinical experience has shown that sensation testing of the area served by the SRN is occasionally affected, resulting in paraesthesias or dysaesthesias. This makes sense as the nervous system is continuous and there is clear evidence of retrograde axonal reflex arcs that result in nerve injuries or irritation.
Imaging
Ultrasound and magnetic resonance imaging (MRI) are the preferred imaging methods to determine the location of the nerve compression of the PIN in the radial tunnel. However, there are currently no gold standard imaging techniques for diagnosis of RTS or PINS. Stevens (2010) reported that findings on MRI for RTS and PINS are identical with oedema or fatty infiltration within the supinator and extensor muscles. There are also reports of neural oedema proximal to the site of compression when observed with ultrasonography (Chien 2003). Further (Ferdinand et al. 2006) retrospectively reviewed 25 patients MRIs who were diagnosed with symptoms consistent with RTS. The regions of compression were varied, with 13 patients having oedema or atrophy within supinator and wrist extensors, four had thickening of the leading edge of ECRB and there was one patient each who had prominent recurrent radial vessels, schwannoma and bicipitoradial bursa. There were also four with normal findings and two with lateral epicondylalgia. Of course, there is a lack of current evidence to determine what is normal in this region, and as we all know, if something is compressed, it isn’t necessarily complaining!
Additional testing
Grip strength testing
Considering the anatomical course of the radial nerve branches and the changes in pressure within the radial tunnel as the wrist moves into pronation, grip strength testing would provide a method of testing the dynamic compression loading of the DBRN or the PIN in the radial tunnel. It seems that no clear pattern exists across different patients, but is related to their provocative activities, ie carrying in supination vs gripping in pronation like the cleaning pictures above.
Neural tissue provocation testing
Neural tissue provocation testing of the radial nerve (ULNT 2b) can also tell you about the sensitivity of the radial nerve, and frequently reproduces pain. Sometimes, combining this test with an isometric grip, such as a tennis ball can assist to induce symptoms in those with only mildly provocative symptoms.

While Radial Tunnel Syndrome and Posterior Interosseous Nerve Syndrome are only in the early stages of investigation in peer reviewed literature, like all good clinicians, a clinical reasoning approach is what provided good diagnosis and management. With good knowledge of the basic anatomy, and relevant clinical testing the clinician can easily diagnose this condition as a differential for lateral elbow pain. Management for nerve related conditions like all musculoskeletal conditions revolves around movement, but the specifics for management in these two radial nerve conditions will differ greatly from the standard management for traditional diagnosis of “Tennis Elbow” – but more on that in a later post.
What are your thoughts? Do you consider this differential diagnosis for lateral elbow pain? What do you think of the examination procedures above? Do you have any additional tests that can further assist with the diagnosis of Radial Tunnel Syndrome and Posterior Interosseous Nerve Syndrome? If so, please comment below, I look forward to a good discussion on this topic.
Jay Tan Physio
References
Bentley FH, Schlapp W. (1943). “The effects of pressure on conduction in peripheral nerve.” Journal of Physiology: 102: 72– 82.
Berton, C., et al. (2012). “The supinator muscle: anatomical bases for deep branch of the radial nerve entrapment.” Surgical and Radiologic Anatomy: 1-8.
Bolster, M. and X. Bakker (2009). “Radial tunnel syndrome: emphasis on the superficial branch of the radial nerve.” Journal of Hand Surgery (European Volume) 34(3): 343-347.
Chien, A. J. (2003). “Sonography and MR imaging of posterior interosseous nerve syndrome with surgical correlation.” AJR, American journal of roentgenology 181(1): 219.
Cleary, C. K. (2006). “Management of Radial Tunnel Syndrome: A Therapist’s Clinical Perspective.” Journal of Hand Therapy 19(2): 186-191.
Crawford, G. (1984). “Radial tunnel syndrome.” The Journal of hand surgery 9(3): 451.
Dang, A. C. and C. M. Rodner (2009). “Unusual compression neuropathies of the forearm, part I: radial nerve.” J Hand Surg Am 34(10): 1906-1914.
Ferdinand, B. D., et al. (2006). “MR Imaging Features of Radial Tunnel Syndrome: Initial Experience.” Radiology 240(1): 161-168.
Hazani R., et al. (2008). “Anatomic landmarks for the radial tunnel.” Eplasty 8(37).
Hsu, S. H., et al. (2012). “Physical examination of the athlete’s elbow.” The American Journal of Sports Medicine 40(3): 699-708.
Huisstede, B., et al. (2006). “Interventions for treating the posterior interosseus nerve syndrome: a systematic review of observational studies.” Journal of the Peripheral Nervous System 11(2): 101-110.
Kleinert, J. M. and S. Mehta (1996). “Radial nerve entrapment.” Orthopedic Clinics of North America 27(2): 305-316.
Lin, Y. T., et al. (2006). “Nerve endings of the wrist joint: a preliminary report of the dorsal radiocarpal ligament.” Journal of orthopaedic research 24(6): 1225-1230.
Lutz, F. (1991). “Radial tunnel syndrome: an etiology of chronic lateral elbow pain.” J Orthop Sports Phys Ther 14(1): 14-17.
Naito, M., et al. (2013). “Simultaneous bilateral posterior interosseous nerve palsy caused by rheumatoid synovitis of the elbows.” Modern Rheumatology: 1-7.
Rempel, D., et al. (1999). “Pathophysiology of Nerve Compression Syndromes: Response of Peripheral Nerves to Loading*.” The Journal of Bone & Joint Surgery 81(11): 1600-1610.
Rydevik, B., et al. (1981). “Effects of graded compression on intraneural blood blow: an in vivo study on rabbit tibial nerve.” Journal of Hand Surgery: 6:3–12.
Roquelaure, Y., et al. (2000). “Occupational risk factors for radial tunnel syndrome in industrial workers.” Scandinavian journal of work, environment & health: 507-513.
Spinner, M. (1968). “The arcade of Frohse and its relationship to posterior interosseous nerve paralysis.” Journal of Bone and Joint Surgery 50: 809-812.
Stevens, K. J. (2010). “Magnetic resonance imaging of the elbow.” Journal of Magnetic Resonance Imaging 31(5): 1036-1053.
Toussaint, C. P. and E. L. Zager (2008). “What’s new in common upper extremity entrapment neuropathies.” Neurosurgery Clinics of North America 19(4): 573-581.
Tsai, P. and D. R. Steinberg (2008). “Median and radial nerve compression about the elbow.” The Journal of Bone & Joint Surgery 90(2): 420-428.
Werner, C., et al. (1980). “Direct recording of local pressure in the radial tunnel during passive stretch and active contraction of the supinator muscle. Archives of Orthopaedic Trauma and Surgery 96: 299-301.



It’s interesting to read. I recently went to a hand therapist who has suggested that I have radial nerve problems and not epicondylitis that has been suggested over 2 yrs by other drs? The things I explained resonated with him and when I read about radial tunnel syndrome, I couldn’t help but think, why has it taken this long and the differences seems so obvious to me. Perhaps I also have epicondylitis?
Treatment may have been different?
Hi Diana,
I am glad you found this post interesting! Hopefully if you do have this condition, you have found someone who considers this condition in the diagnosis of pain in the outer elbow. Lateral epicondylalgia (formerly epicondylitis), is by far the most common diagnosis in this region, which accounts for many health providers missing the diagnosis of Radial Tunnel Syndrome. The two conditions do occur very frequently together. I usually have the feeling that if the radial nerve which serves the tissue on the outer elbow is presensitised, then the traditional rehabilitation for epicondylalgia – resistance loading will likely fail.
Treatment for nerves includes different exercises, including nerve gliding exercises which a good physio can advise you on. I had planned to write another post on the management of this condition, but have been very busy as of late. Thanks for the reminder, and I’ll get back to blogging. Stay tuned for the update on “Management for Radial Tunnel Syndrome and Posterior Interosseous Nerve Syndrome”.
Regards,
Jay Tan Physio
Thanks for this article, after over a year of searching for an explanation for my pain other than epycondilitis I feel that finally I found an acceptable diagnosis. It describes exactly what I feel and I will take this up with my doctor. Would love to read more about the management of this condition!
Yours Truly,
Kjell
I found this article be extremely interesting. I recently fell and broke my left wrist which was repaired with plates and screws. After a four month recovery period, I now find that I have a tingling sensation running from my wrist and revolving around my elbow and then moves up to my shoulder. I am currently having physical therapy but haven’t found any relief. I work as a letter carrier and my job requires me to lift lots of weight and now notice that the sensations are exacerbated when I lift my arm past my shoulder. I plan to print this article to show to my therapist, hoping that it might help in diagnosing my issue. Excellent article.